The Expanding Role of Digital Health Technology Suites in Modern Healthcare
Digital health technologies (DHTs), encompassing mobile health (mHealth) applications, telehealth platforms, and wearable devices, are experiencing increased adoption worldwide. However, their integration into medical practice varies significantly across nations, particularly concerning regulatory approval, reimbursement, and overall perception.
DHTs offer the potential to enhance the affordability and sustainability of healthcare, addressing previously unmet societal needs by providing customized care solutions. This capability facilitates both safer and more accessible home-based care while empowering patients to actively engage in their own health management.
This article, the first in a two-part series, explores the emergence of flexible DHT suites, examines existing regulatory and Health Technology Assessment (HTA) frameworks, and analyzes their application within the context of the COVID-19 pandemic. The subsequent article will delve into potential new regulatory frameworks.
The Emergence of DHT Suites
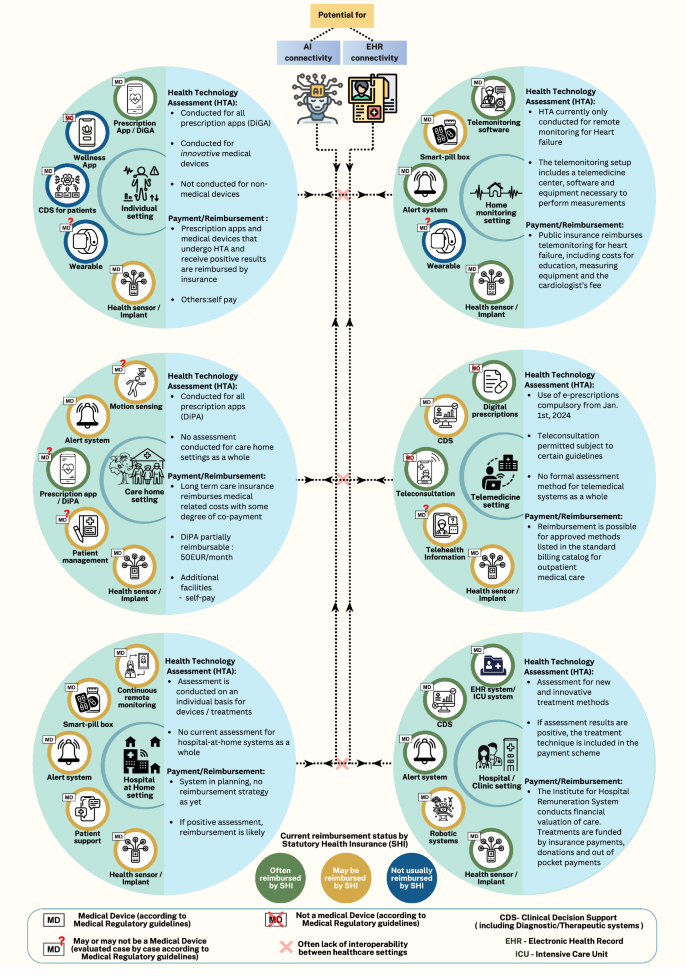
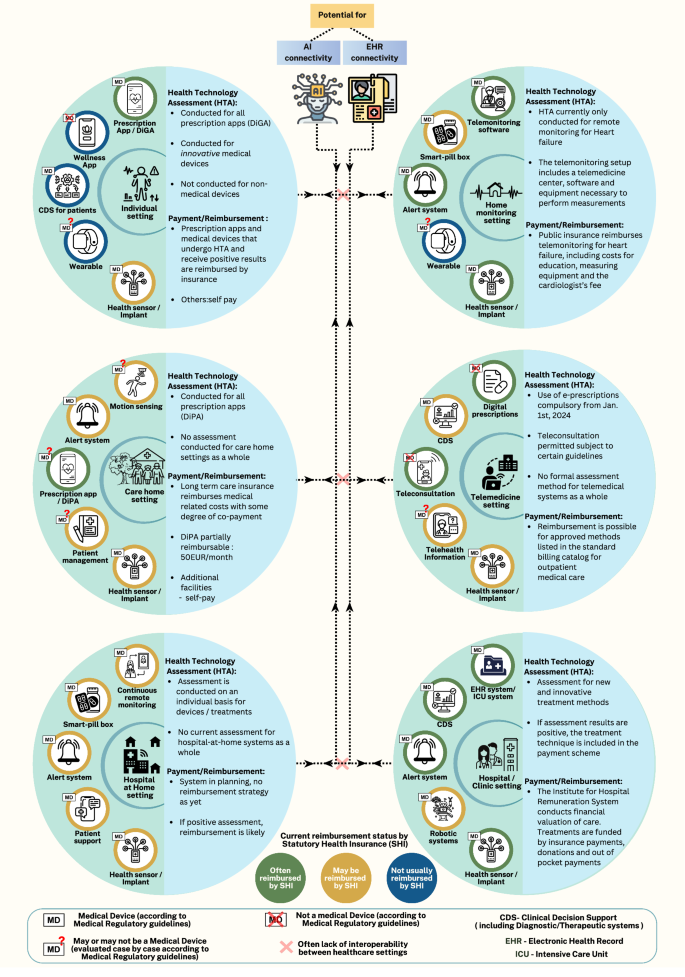
The COVID-19 pandemic accelerated the bundling of individual DHTs—each with a specific medical purpose and associated approvals—into comprehensive suites designed to deliver aggregate ‘intended purposes.’ These purposes sometimes differ from those of the individual components. The complex interactions within and between these suites present new paradigms of medical treatment. These devices, with various levels of workflow integration with telemedicine systems and electronic health records (EHRs), can also produce unexpected outcomes.
Services delivered via device-aggregates encompass remote passive and active sensor systems, automated monitoring platforms, and teleconsultation tools to:
- Enable healthcare providers (HCPs) to monitor chronically ill patients at home.
- Facilitate Hospital-at-Home (HaH) programs.
- Improve treatment efficiency in hospital and care home settings.
-
Enable ‘smart clinics’ with patient evaluations performed remotely by clinicians via mHealth platforms and devices like wireless thermometers and stethoscopes.
The implementation, evaluation, and assessment of interactions within these grouped systems of networked devices pose unique challenges, particularly for regulatory and health technology assessment (HTA) purposes.
The Grouping of Medical Devices: A Historical Perspective
While the grouping of separate medical devices predates DHTs, a key difference is that DHTs are used to build suites of networked devices, which have complex data flows and subsequent dynamic dependencies. Although many suites continue to rely on healthcare staff for operation, there is a realistic potential for transitioning to greater automation and use of these aggregations as ‘super devices’ with limited human intervention in the future.
Hospital-at-Home: A Case Study of DHT Evolution
The Hospital at Home (HaH) model typically consists of aggregated health sensors, alert systems, remote monitoring platforms, and systems for digital patient support. The HaH concept existed before the COVID-19 pandemic but gained more traction during the pandemic, due to temporary regulation and reimbursement changes.
In the US, the Centers for Medicare and Medicaid Services (CMS) allowed for the reimbursement of HAH care as a diagnosis-related group (DRG) and waived some remote patient monitoring requirements. Other regulatory changes encouraged telehealth adoption, remote data acquisition, and accelerated trial processes.
Countries that have adopted the HaH model include the UK, US, Spain, The Netherlands, Canada, and Australia, with early adoption in many other European countries. In February 2024, the CMS extended the acute HaH program, initiated in 2019 during the pandemic, until the end of 2024 to further evaluate the benefits of HAH, marking a pioneering step towards telehealth adoption. A 2023 early value assessment by the National Institute for Health and Care Excellence (NICE) in the UK supported the potential cost-effectiveness of HAH or virtual wards. That review also highlighted assessment challenges such as insufficient prior data, a lack of suitable comparators, interactions across diverse policies, variations in the standard of care, and overall heterogeneity, however, NICE’s conditional approval supported both the ability to safely generate further evidence and the addressing of unmet patient needs.
Challenges for Adoption and Evaluation
The grouping of DHTs presents safety and performance challenges due to device interactions and emergent system properties, particularly when incorporating both medical and non-medical devices. Ensuring interoperability across various demographics and settings requires thorough examination of each system component. Furthermore, the cybersecurity of both individual components and the entire DHT suite, including Internet of Medical Things (IoMT) devices, warrants careful regulatory attention, especially for systems forming a clinical health delivery infrastructure such as HaH. Many DHTs are adaptive, through software refinements or AI training, bringing additional complexity to the regulatory landscape.
In the EU, medical device regulations mandate that systems of medical devices (MD) and non-MD DHTs are treated as MDs by regulatory authorities. The commercial provider is obliged to risk assess all components, providing clinical data for the combination. The interpretation of EU law appears to suggest that manufacturers incorporating smartphone/smartwatch components might require MD approval for all components, even those they don’t produce, which is difficult given their non-manufacturer status. Reimbursement of DHT systems is also challenging. Assessing cost-effectiveness and gathering evidence for extensive modular DHT suites introduces complexities, including the scarcity of comparators and the complex estimation of initial investments.
Conclusion
The future benefits of DHTs in driving quality and efficiency in healthcare will rely heavily on the use of digital health technology suites. In the US, the Center for Devices and Radiological Health (CDRH) is working on forward-thinking regulatory pathways. The concept of DHT suites will continue to mature, along with economic evaluations. While temporary adaptations of HTA frameworks worked well during the pandemic, there’s an opportunity to explore how new frameworks and paradigms can be developed for complex multi-device digital/human workflows. The second article in the series will delve into what new frameworks could include.